The fee-for-service payment scheme used in healthcare is problematic as it prioritizes quantity over quality, leading to overutilization of services and escalating costs while hindering the possibility of focusing on improving the quality of care.
Recognizing this challenge, the Institute for Healthcare Improvement (IHI) conceived the idea of the Triple Aim, outlining key strategies for enhancing healthcare delivery.
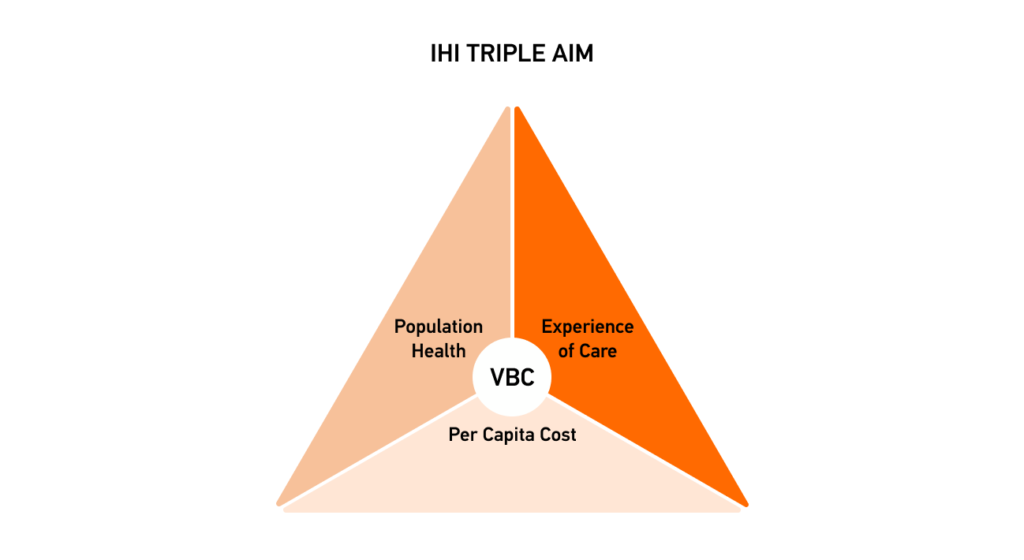
Moving towards value-based care requires digitization and seamless exchange of healthcare data.
This transition aims to reduce costs by avoiding unnecessary hospital admissions, relying on primary care for routine needs, and managing various resources accurately (e.g., prescriptions, imaging services, labs, diagnostic coding, etc.).
However, the complexities caused by the intricacy of healthcare data flow may include errors during data aggregation and analysis, reducing the accuracy and efficiency of insights crucial for providing quality care.
The Da Vinci Project is one of the initiatives that have been working on ensuring smooth data flow and establishing effective cooperation between various healthcare stakeholders.
Overview of the Da Vinci Project: its Role in Interoperability and Value-Based Care
The Da Vinci Project is part of the FHIR Accelerators program, designed to assist healthcare communities with FHIR Implementation Guides (IGs) to ensure the global adoption of the Fast Healthcare Interoperability Resources (FHIR) standard, designed by the Health Level 7 organization to support healthcare stakeholders with means for achieving global health data interoperability.
Da Vinci aims at uniting payers, providers, and pharmaceutical companies to explore shared challenges using FHIR and interoperability. A fundamental component in this process is the utilization of FHIR bundle, which facilitates the efficient grouping and exchange of healthcare data.
Read also: FHIR vs HL7: Main Differences
Why FHIR?
- FHIR (Fast Healthcare Interoperability Resources) is a standardized healthcare data exchange framework developed by the HL7 (Health Level 7) organization;
- Open Source and Free;
- It provides a modern, web-based approach to interoperability in healthcare:
– RESTful API
– XML and JSON
- Resources as the building blocks of healthcare and life sciences data;
- HL7 FHIR is increasingly being adopted in the life sciences industry as well.
DaVinci primarily focuses on enhancing value-based care and facilitating seamless data exchange by ensuring the wide adoption of the FHIR standard. They define requirements, develop implementation guides, and pilot solutions to advance value-based care initiatives.
How does Da Vinci Solve Interoperability and Cooperation Problems in Healthcare?
The Da Vinci healthcare initiative leads collaborative efforts to solve interoperability challenges by ensuring multi-stakeholder engagement, involving top talent when developing interoperability strategies, and delivering high-impact, implementable solutions. They are cooperating with the ONC’s P2 FHIR Task Force to promote FHIR adoption in a way that supports value-based care initiatives.
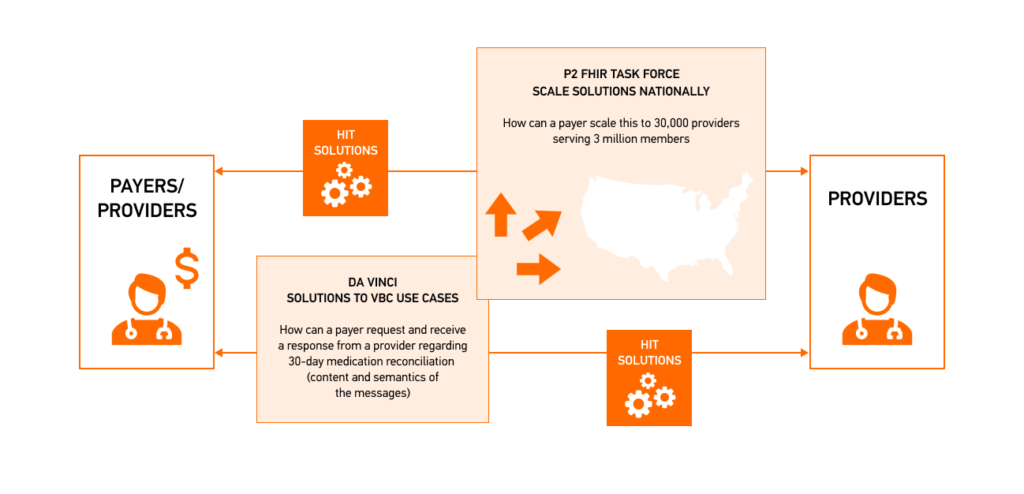
The Payer-Provider (P2) FHIR Task Force tackles issues such as security, scalability, identity management, and exchange process. At the same time, the DaVinci Project targets use cases from the perspective of VBC by creating solutions that minimize the need for developing and deploying unique solutions for various healthcare use cases.
Da Vinci’s Approach to FHIR Implementation
With ongoing input from stakeholders in the Da Vinci Project, new use cases are continuously added and assessed by the project’s committees.
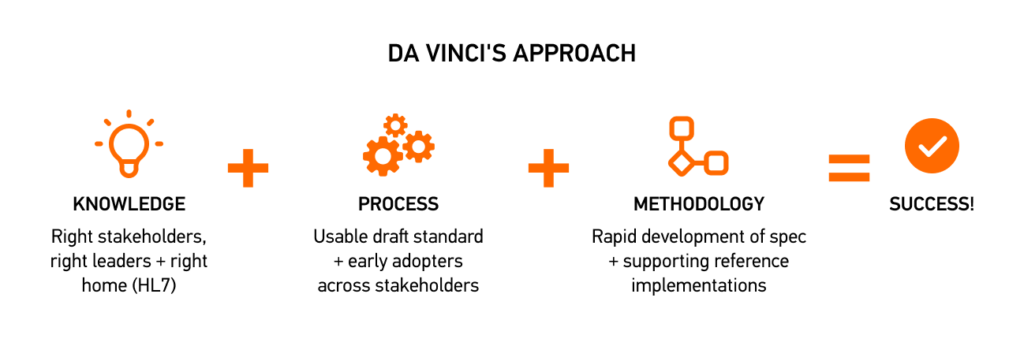
Da Vinci’s Implementation Guides are designed to integrate FHIR into everyday healthcare practices and transition to the VBC model.
| FHIR DaVinci IG Name | A Brief Description |
| Data Exchange Quality Measure | The DEQM IG specifies a framework for automatic data collection and submission that is needed to reduce reliance on manual processing and intervention. IG’s components: • Framework: FHIR transactions and general description. • Use Cases: DEQM implementation scenarios. • Profiles and Extensions: Defined profiles and extensions. • Capability Statements: FHIR capabilities for DEQM actors. • Examples: Examples used in the guide. The guide describes FHIR transactions and profiles that stakeholders can use to enable seamless communication between systems involved in quality measure reporting. |
| Coverage Requirement Discovery | The CRD IG presents a process enabling payers to convey coverage requirement information to providers through their clinical systems. Key Ideas Behind the IG: • CRD Clients: Provider systems(e.g., EHRs, pharmacy systems, etc.) may comprise multiple interconnected systems and require coverage requirement data for care planning. • CRD Servers: Payers systems share coverage information with providers. FHIR establishes a standardized framework for sharing coverage requirement information, documentation rules, and authorization requirements between CRD Clients and Servers, ensuring efficient and accurate data exchange. |
| Documents, Templates & Rules | The DTR IG describes the payers’ approach to communicating documentation requirements to providers through their clinical systems. Key points: • DTR IG compliments the CRD and other Da Vinci FHIR IGs. • The guide allows for leveraging FHIR Questionnaires and Clinical Quality Language logic to facilitate extracting and submitting relevant documentation information. FHIR-based frameworks and standardized protocols enable accurate exchange documentation between payers and providers, ensuring that providers have access to the context-specific documentation requirements during critical care procedures. |
| Prior Authorization Support | The PAS IG describes the mechanism of obtaining approval from payers (such as insurance companies) before delivering specific care or treatments to patients. Key points: • The Prior Authorization (PA) Workflow involves assessing the need for approval, gathering patient data, submitting requests, monitoring status, and updating information when necessary. • This guide implies using such technologies as: – FHIR API (for data exchange between different systems) – CDS Hooks (for verifying payer coverage and determining the need for prior authorization). Delivering the authorized treatment to the patient ensures the coverage of treatment plans that help control healthcare costs and prevent unnecessary treatments. |
| Clinical Data Exchange (CDex) | The IG describes implementing FHIR-based interactions to facilitate specific clinical data exchanges between providers and payers or other providers. Key Scenarios Supported by the CDex IG: • Requesting and Sending Attachments (for claims and prior authorization); • Documentation Requests for Payer Operations (e.g., claims audits); • Gathering Quality and Risk Adjustment Information; • Exchanging clinical data between referring providers. By using this IG, providers can efficiently articulate data requests and ensure the transmission of only the necessary information, enhancing data exchange accuracy and fostering cooperation between payers and providers. |
| Health Record Exchange Framework | HRex is a foundational resource for all DaVinci IGs, defining FHIR profiles and operations for various use cases, including data exchange between US payers and providers under HIPAA guidelines. The IG dependencies: • Based on the FHIR R4 specification; • Leverages US Core Implementation Guide wherever possible (particularly the US Core 3.1 IG); • Complies with the Quality Improvement Core (QI-Core) IG. • Uses components from other FHIR-related IGs, including Bulk Data, C-CDA on FHIR, CDS Hooks, CQL, FHIRPath, SMART on FHIR. Adherence to established standards and IGs promotes consistency, reliability, and interoperability while exchanging data between actors and streamlining the processes by ensuring compatibility with existing healthcare standards and technologies. |
| Payer Data Exchange | The PDex IG provides means for creating Member’s Health History using clinical data based on US Core Profiles so Payers/Health Plans could understand and integrate the information into Electronic Medical Records (EMR) Systems. Key points: • The guide is based on the HL7 FHIR 4.0.1 standard; • The IG covers three methods of information exchange: CDS-Hooks and SMART-on-FHIR, OAuth2.0 or SMART-on-FHIR Member-authorized Exchange, and $patient-everything Exchange operation via Alternate Secure Transport; • The guide introduces a Provenance resource, essential for ensuring data traceability, which Health Plans shall include in all FHIR data exchanges to identify the source of information. |
| Payer Coverage Decision Exchange | The PCDE IG is designed to facilitate the exchange of coverage-related information, such as the “current active treatments” from a prior payer to a new payer, to minimize care interruptions and enhance patient safety and experience. Key Components and Dependencies: • The IG relies on FHIR R4, Da Vinci HRex, and Da Vinci PDex IGs. • The PCDE IG provides a structured framework for payers to communicate essential information, such as active treatment plans, clinical conditions, guideline evaluation, prior authorizations, treatment history, and clinical documentation. The standardized exchange of the information described above ensures that providers access relevant and up-to-date data, facilitating seamless care coordination and informed decision-making. |
| Patient Cost Transparency (PCT) | DaVinci’s PCT IG provides guidance on using FHIR-based standards to facilitate the exchange of financial information between providers and payers. It enables providers to submit Good Faith Estimates (GFEs) to payers and subsequently generate Advanced Explanations of Benefits (AEOBs) for patients, which allows them to manage their healthcare expenses. Key Components: • Workflows (GFE Request and Collection Workflow and GFE Submit Workflow. These workflows enable providers to request, collect, and submit GFEs to payers required to generate AEOBs for patients.) • Actors: – Business Actors: Patients, Convening Providers, Co-Providers, and Payers (business actors responsible for collecting and sharing GFEs and AEOBs, ) – Technical Actors: GFE Requesters, GFE Contributors, Coordination Platforms, and GFE Submitters (perform specific actions in workflows to ensure that the exchange of GFEs and AEOBs happens as described in the guide.) This IG allows healthcare stakeholders to establish standardized methods for predicting patient expenses. |
| Risk Adjustment | The RA IG provides standardized risk adjustment data communication protocols to explain how risk adjustment coding gaps are exchanged between payers and providers. Key Components: • Methodology (defines resource profiles and operations, outlines steps for generating reports, querying data, submitting evidence, and utilizing digital categories to ensure consistency in implementation.); • FHIR Artifacts (specific resources like profiles, extensions, and operations required for exchanging risk adjustment coding gaps.). FHIR facilitates the standardized exchange of risk adjustment coding gap data between payers and providers, ensuring seamless communication and interoperability to address coding gaps in risk adjustment documentation. |
| Value Based Performance Reporting (VBPR) | The VBPR IG facilitates the exchange of financial and quality performance data between payers and providers through performance reports. Key Components of VBPR Reports: • Performance Categories (evaluate provider performance in clinical quality, cost, utilization, and patient experience); • Quality Measures (assess clinical outcomes, patient safety, and adherence to best practices); • Performance Benchmarks (compare provider performance to industry standards); • Incentive Payments (reward or penalize based on performance to improve care quality); • Risk Adjustment (adjust for differences in patient populations to ensure fair comparisons). The VBPR IG allows for evaluating healthcare provider performance within value-based contracts, which aim to enhance care quality, patient outcomes, and cost efficiency by rewarding performance over service quantity. |
As you can see, all of the DaVinci FHIR Implementation Guides are aimed at providing a framework for stakeholders to make a shift from fee-for-service to value-based care (VBC), which is undoubtedly going to shape the future of health IT and support a variety of healthcare use cases.
| Real-World Use Cases of DaVinci IGs Implementation | |||||||
| Project | A Brief Description | ||||||
| FHIR for medication data sharing | Goal: To improve medication data sharing between providers and payers. Description: This project focused on Medication Reconciliation Post-Discharge (MRP) when implementing FHIR use cases for Data Exchange Quality Measure (DEQM) to complete the medication reconciliation and reduce manual steps for stakeholders involved in this process (MultiCare and Regence). Result: • Improved medication reconciliation for 62% to 66% of patients; • Reduced staff time by 5 to 10 minutes per patient for MultiCare; • Eliminated manual intervention for Regence;cost reduction. | ||||||
| FHIR-based information exchange | Goal: To establish an API-enabled approach for information transfer. Description: • Implemented the Payer Coverage Decision Exchange (PCDE) use case to facilitate the FHIR-based exchange of clinical data between old and new payers; • Enabled the transfer of “current active treatments” from the prior payer to the new one; • Reduced the need for providers and patients to resubmit supporting documentation for ongoing treatment. Result: The PCDE scheme ensures a smooth transition and prevents disruptions in care plans and medication adherence by enabling FHIR-first exchange and minimizing human intervention when transferring essential information like current treatments, diagnoses, clinical guidelines, prior authorizations, and supporting documents. | ||||||
| FHIR for gathering lab results | Goal: To facilitate the ability to gather lab results for members and close gaps in clinical quality measures. Description: The CDex use case was employed to track HbA1c levels (which measure average blood sugar) in diabetic patients by triggering a “lab chase” query upon receiving a claim, which was sent to the lab vendor’s FHIR server to check for available lab results. Result: The CDex implementation improves data retrieval efficiency by enabling FHIR-based queries for lab results to be processed in near real-time. Hence, relevant clinical data can be accessed without delays, allowing for faster decision-making and interventions when necessary. | ||||||
If any of the use cases described in the FHIR Da Vinci IGs sound relevant to your project and you want to know more about leveraging the FHIR standard to jump on the VBC train, do not hesitate to get a consultation from our certified experts and developers of ONC and HIPAA-compliant Kodjin FHIR Server.
Our FHIR developers have a proven track record of overcoming the challenges of healthcare interoperability by implementing FHIR for startups to meet our client’s expectations and the ever-changing regulatory requirements.
FAQ
What is the DaVinci Project?
Da Vinci is a US-based project that fosters collaboration among key healthcare stakeholders, such as providers, payers, vendors, etc.
What is the difference between DaVinci and HL7?
HL7 is a nonprofit organization that develops standards, including the HL7 FHIR standard for interoperability, while DaVinci is one of the HL7 Accellerator’s Program representatives that promote the implementation of the FHIR standard in the US.
How does the Da Vinci Project solve cooperation problems in healthcare?
Da Vinci ensures multi-stakeholder engagement by involving top talent when developing interoperability strategies and FHIR implementation guides.