Key Takeaways:
- Mapping healthcare data to HL7 FHIR resources is crucial for seamless communication and interoperability in the healthcare industry, mandated by the 21st Century Cures Act.
- Effective FHIR mapping automates the process of converting diverse clinical data into standardized formats, reducing manual effort and increasing consistency across healthcare systems.
- Our custom FHIR resource mapper simplifies the complex and time-consuming process of transforming clinical data into FHIR-compliant formats, enhancing efficiency and accuracy.
Mapping healthcare data to HL7 FHIR resources is crucial for achieving seamless communication and interoperability in the healthcare industry. Also mapping healthcare data to HL7 FHIR resources requires a deep understanding of the HL7 FHIR Data Model, which provides the foundation for structuring and exchanging health information.
Many healthcare organizations operate independently, which creates challenges for data processing and exchange. FHIR specifications aim to solve this issue by standardizing the way data is stored in health systems, thus enabling seamless healthcare data exchange. In fact, with the 21st Century Cures Act going into effect, FHIR adoption has already become mandatory for healthcare organizations in the US.
However, given the complexity, diversity, and volume of the clinical data aggregated by healthcare organizations, FHIR implementation becomes a difficult and time-consuming process. One of the biggest issues is HL7 to FHIR mapping, which is essential to achieve compliance and ensure seamless data transformation.
Having worked on multiple large-scale FHIR projects, our team has developed a custom FHIR resource mapper that transforms any clinical resource into a FHIR data mapping format. In this article, we want to share the issues we were able to solve for our clients and how we did it. We will also illustrate the FHIR mapper’s capabilities with JSON examples to provide a better understanding of its functions and how to map a resource in FHIR.
What is HL7 FHIR?
Fast Healthcare Interoperability Resources (FHIR) is an open standard developed by the HL7 International organization to facilitate seamless exchange of electronic health data between different healthcare systems and promote interoperability.
Read Also: FHIR vs. HL7: What to Choose
FHIR was built on modern web technologies such as REST API, JSON and XML, which makes it easier for developers to implement and use. It utilized a resource-based data model for representing healthcare data. Each HL7 FHIR resource corresponds to a specific element of healthcare data such as a patient, medication, or clinical observation. This modular approach enables flexible and granular exchange of data, and allows for easier EHR systems integration.
The standard has gained widespread adoption in the healthcare industry, and is supported by major EHR vendors, healthcare providers, and government agencies. It is seen as a key enabler of interoperability and data exchange in healthcare, and is expected to play a major role in advancing healthcare technology and improving patient care. Effective mapping to FHIR resources not only improves data accuracy but also enhances interoperability through HL7 Integration, allowing different systems to communicate effortlessly.
Read also: Introduction to FHIR Data Model
What is a Healthcare Data Mapping & FHIR Mapper?
Are you wondering what is data mapping in healthcare? Whenever you need to match fields from one database to another, you “map” the data. In the case of the FHIR specification, you map the data you have to FHIR resources.
For example, we have a Patient resource stored in a database in a particular format, but you need to have it in a FHIR format. You could hire a team of data analysts to do so manually, but that would be an immensely time- and cost-consuming task. Instead, you could automate the process of clinical data mapping to a FHIR resource by using a FHIR mapper.
How we built a FHIR mapper
We built a custom FHIR mapper that utilizes resource templates. Data analysts can easily customize these templates however is needed. For example, there’s a deleted_date field we deleted in one template; however, later on, we needed that field in another template. A data analyst can add said field by just writing a few lines in the JSON template.
The process of transforming a custom resource into a FHIR structure
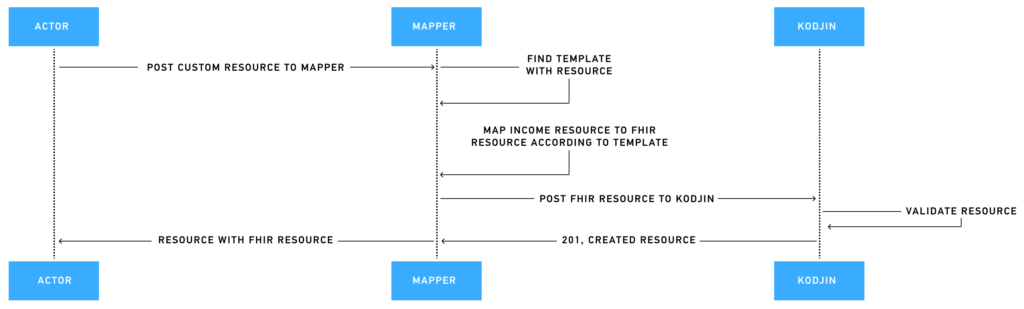
Our FHIR mapping tool utilizes various functions to map one resource onto another. Below we’ll take a look at these functions and provide some examples for better understanding.
_if mapping function
The keyword _if checks whether the field exists in the incoming JSON code. This validation is used for the cases when a JSON block has static fields along with data from the incoming JSON. For example, in the next block we check whether Patient in the incoming JSON code has ethnicity. If it doesn’t have the entire block, it will be absent in the outcoming JSON code.
{
"_if": "{Patient.ethnicity}",
"extension": [
{
"url": "ombCategory",
"valueCoding": "{Patient.ethnicity|ethnicity_code}"
},
{
"url": "text",
"valueString": "{Patient.ethnicity}"
}
],
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-ethnicity"
}
_ifnot mapping function
The keyword _ifnot is applied when data is absent in the incoming resource. For example, let’s take a look at the valueQuantity in the Observation resource. If data for Patient weight is present, the Observation resource will include valueQuantity data listed in the incoming resource; if not, an absence reason will be listed (e.g., “value was not set by Doctor”).
"valueQuantity": {
"_if": "{Patient.weight.value}",
"value": "{Patient.weight.value|float}",
"unit": "{Patient.weight.units}",
"system": "http://unitsofmeasure.org",
"code": "[lb_av]"
},
"dataAbsentReason": {
"_ifnot": "{Patient.weight.value}",
"text": "value was not set by Doctor"
}_foreach mapping function
The keyword _foreach creates FHIR HL7 resources in the outcoming resource for each object or element in the array element from the incoming resource.
{
"phones": [
{
"phone": "4155555555",
"phone_type": "Home",
"created_date": "2016-10-10T23:31:49",
"deleted_date": null
},
{
"phone": "5155555555",
"phone_type": "Main",
"created_date": "2016-10-10T23:31:49",
"deleted_date": null
}
]
}In this case, we’ll create a telecom element for each object in the phones array.
{
"telecom": [
{
"_foreach": "{Patient.phones}",
"use": "{array_element.phone_type|phone_type_to_use}",
"system": "{array_element.phone_type|phone_type_to_system}",
"rank": "{array_element.phone_type|phone_type_to_rank}",
"value": "{array_element.phone}",
"period": {
"start": "{array_element.created_date}",
"end": "{array_element.deleted_date}"
}
}
]
}_flatten mapping function
Sometimes incoming FHIR resources could have arrays with arrays, and you need to map the data from the first array element to the second one.
For example, we have custom_report_income_resource.
{
"id": "123",
"patient": "456",
"report": [
{
"report_id": "number_1",
"resulted_date": "2022-10-13T09:37:00Z",
"collected_date": "2022-10-13T09:37:00Z",
"note": "this is a note",
"results": [
{
"status": "FINAL",
"value": "12",
"units": "%",
"observation_code": {
"name": "Hematocrit",
"loinc_code": "4544-3"
}
}
]
}
]
}For each report element, we will create a Diagnostic report resource, and for each report.results, we will create an Observation resource. Data for each observation is in the report resource. For this case, we use _flatten, and we refer to the above element through report{array_element_above.#}.
Terminology mapping
The examples below show HL7 mapping between incoming codes and outcoming codes. The block is for the AllergyIntolerance resource. DrugIntolerance.status is incoming data and contains a list of codes.
{
"clinicalStatus": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/allergyintolerance-clinical",
"code": "{DrugIntolerance.status|drug_intolerance_status}"
}
]
}
}We save separate mappings for such lists. For example:
{
"drug_intolerance_status": {
"1": "active",
"2": "inactive"
}
}As such, by using this type of HL7 mapping, we could use code from terminology.
Benefits of FHIR-Based Healthcare Interoperability
Below, we will explore some of the advantages the FHIR standard provides for healthcare interoperability.
Improved Data Exchange
FHIR’s standard format and protocol facilitate efficient and standardized data exchange between healthcare organizations. This standardization minimizes data translation errors and improves patient outcomes by ensuring that all parties have accurate and up-to-date information.
Easier integration with third-party systems
FHIR’s use of RESTful APIs simplifies the integration with other healthcare IT systems. This enables seamless coordination of care across different providers and systems, enhancing the overall quality of healthcare delivery and ensuring that patient information is accessible whenever and wherever it is needed.
Better Clinical Care
Access to Electronic Health Records (EHRs) by medical personnel and the hassle-free integration of these records in software applications significantly improve patient care. It enhances safety, effectiveness, timeliness, efficiency, and equity in healthcare delivery. This comprehensive access to patient data ensures that clinicians can make informed decisions quickly.
Read also: EHR interoperability: Importance, Issues, and Solutions
Enhancement in Data Management
Standardized data format simplifies and optimizes data management by providing solutions and choosing necessary FHIR tools to manage the significant volume of available data. Harmonized data ensures data integrity, accuracy, and consistency, and minimizes poor-quality data.
Holistic Patient Experience
The interoperability offered by the FHIR standard provides patients control over the use and monitoring of their data, thus empowering them and allowing for a more holistic patient experience. Patients can choose how and what information they share with healthcare providers, thus increasing faith in the industry and giving them power over the decisions of their treatment.
Compliance with Regulations
FHIR-based interoperability solutions assist healthcare organizations in complying with regulatory requirements, such as HIPAA and the ONC Interoperability Rule. By ensuring that data exchange meets these standards, organizations can avoid legal issues and maintain patient privacy and security.
Simplified Development
FHIR leverages modern web technologies and standards, making it easier for developers to create and implement healthcare applications and systems. This simplicity reduces development time and costs, enabling faster deployment of innovative healthcare solutions.
6 Use Cases for Healthcare Data Mapping
Healthcare data mapping is essential for achieving interoperability and seamless integration within healthcare systems. By leveraging FHIR standards, organizations can ensure efficient data exchange, improved patient care, and compliance with regulatory requirements. Mapping specific patient information often involves creating a FHIR patient profile, which defines the structure, constraints, and data elements for individual patient records to ensure consistent and interoperable healthcare data exchange. Below are key healthcare data mapping use cases demonstrating the broad applicability and benefits adopting FHIR.
1. EHR Integration and Health Information Exchange (HIE)
FHIR for legacy EHR integration ensures seamless conversion of outdated formats, mapping legacy data to FHIR standards and enabling real-time interoperability, efficient data exchange between healthcare organizations. This unified view of patient data improves care coordination and continuity.
2. Clinical Decision Support Systems (CDSS) and Remote Patient Monitoring
By standardizing data to FHIR, CDSS can analyze patient information more effectively, providing evidence-based recommendations. Similarly, mapping data from remote monitoring devices ensures compatibility with EHR systems, supporting continuous patient monitoring and timely intervention.
3. Public Health Reporting and Population Health Management
FHIR data mapping streamlines reporting to public health agencies and supports population health initiatives by enabling the aggregation and analysis of large datasets. This helps manage public health concerns and implement preventive care strategies.
4. Research, Clinical Trials, and Personalized Medicine
Standardized FHIR data facilitates the aggregation and sharing of clinical trial data and genomic information. This supports medical research, precision medicine initiatives, and personalized treatment plans.
5. Telehealth Services and Patient Data Portability
FHIR-based data mapping ensures compatibility of telehealth data with EHR systems, supporting comprehensive patient records. It also enables patient data portability, allowing easy transfer of health records between providers.
6. Medication Management, Billing, and Claims Processing
Standardizing medication data to FHIR improves reconciliation processes, reducing errors and adverse interactions. FHIR mapping also standardizes billing and claims information, enhancing the accuracy of financial transactions and reducing administrative burden.
Challenges of Data Mapping in Healthcare
Healthcare data mapping is critical for achieving interoperability, improving patient care, and enhancing operational efficiency. However, it involves numerous challenges that must be addressed to ensure accurate and meaningful data transformation. Below we will outline key healthcare data mapping challenges and their respective impacts:
| Challenge | Description | Impact |
| Data Standardization | Healthcare data originates from various sources in different formats and terminologies. | Inconsistent data formats can lead to incorrect mapping, data loss, or misinterpretation of clinical information, affecting patient care and operational efficiency. |
| Semantic Interoperability | Ensuring consistent meaning of data across systems due to different coding systems and clinical terminologies. | Semantic inconsistencies can lead to errors in clinical decision support, reporting, and research. |
| Data Quality and Integrity | Maintaining accurate and complete data during transformation is critical. | Compromised data quality can affect patient safety, clinical decisions, and regulatory compliance. |
| Privacy and Security | Protecting sensitive healthcare data throughout the transformation process. | Ensuring compliance with privacy regulations and safeguarding against data breaches is challenging and requires robust security measures. |
| Performance and Scalability | Efficiently transforming large volumes of healthcare data in real-time. | Performance bottlenecks and scalability issues can affect the timeliness and availability of data, impacting clinical workflows and patient care coordination. |
| Legacy Systems Integration | Integrating data from legacy systems that were not designed for modern interoperability standards. | Customization and ongoing maintenance are required to transform and integrate data from legacy systems into FHIR-compliant formats. |
Conclusion
Non-standardized and legacy data formats are one of the biggest obstacles standing in the way of true healthcare interoperability. Understanding the nuances between HL7 and FHIR is crucial for modernizing these systems. However, data mapping in healthcare is not an impossible problem, as we have proved by developing an easy-to-use tool for data mapping to HL7 FHIR.
Mapping healthcare data to FHIR resources is a crucial step in modern healthcare interoperability. For a deeper dive into the intricacies of FHIR, the Ultimate Guide – What is FHIR is a valuable resource for healthcare professionals.
We hope this showcase of our FHIR HL7 mapping solution to the challenge healthcare organizations often face will make FHIR adoption less of a hassle for you. Our HL7 mapping software is one of many our team has created to help clinical data analysts make working with FHIR resources more efficient.
Check out our free low-code FHIR Profile Editor or request a demo of the Kodjin FHIR Server to discover more of the powerful features we offer for FHIR adoption.
FAQ
Why is mapping healthcare data to HL7 FHIR resources important?
Mapping healthcare data to HL7 FHIR resources enables systems to communicate and exchange information in a standardized format, improving interoperability and allowing for better patient.
What are some challenges of mapping healthcare data to HL7 FHIR resources?
Some challenges of mapping healthcare data to HL7 FHIR resources include data mapping errors, inconsistent data formats, and lack of standardized data definitions.
Is data mapping in healthcare secure and compliant with privacy regulations?
Data mapping in healthcare can be secure and compliant with privacy regulations if proper measures are taken. Security and compliance depend on the implementation of robust protocols, such as data encryption, access controls, and regular audits. Additionally, adhering to regulations like HIPAA in the U.S. or GDPR in Europe is essential.
What is the difference between data mapping and data transformation?
Data mapping and data transformation are often used interchangeably because they are closely related processes in the data integration workflow.
If strictly speaking data mapping aligns data elements from a source system to a target system to ensure consistency and interoperability, such as mapping patient demographic fields from one EHR system to another. Data transformation, on the other hand, converts data from one format or structure to another to meet the target system’s requirements.