Key Takeaways
- FHIR includes resources, profiles, implementation guides, and data types, each playing a critical role in structuring, customizing, and securely exchanging healthcare data.
- Resources are the building blocks of the FHIR standard. They cover about 80% of healthcare data needs, with the remaining 20% customized through profiling.
- Profiling of resources allows the extension or constraint of base resources to meet specific use cases.
- FHIR Implementation guides provide rules and guidelines for resource usage, API features, and terminologies, ensuring compliance with national standards and enhancing interoperability.
At the forefront of challenges healthcare organizations face now is data interoperability. Healthcare data has remained fragmented because of different data standards and systems used by individual healthcare organizations. But FHIR has revolutionized this by enhancing interoperability. If you want to understand FHIR components and resources, you are in the right place.
We will take a deep dive into what makes up the FHIR specification, provide examples of resources such as the patient FHIR resource, and demonstrate how Kodjin FHIR Server and our team’s expertise can help streamline your healthcare data integration efforts. With extensive experience in developing and implementing FHIR-based solutions, Kodjin is well-equipped to address your interoperability challenges and enhance your data exchange processes.
FHIR Resources
What are HL7 FHIR resources? Resources are the foundation of the FHIR standard. They are the main structural element of FHIR solutions and are also often referred to as the “building blocks” of FHIR. Each block (resource) is defined by its particular context and contains various healthcare information represented in a standardized way.
Read also: FHIR vs HL7: Which is the best
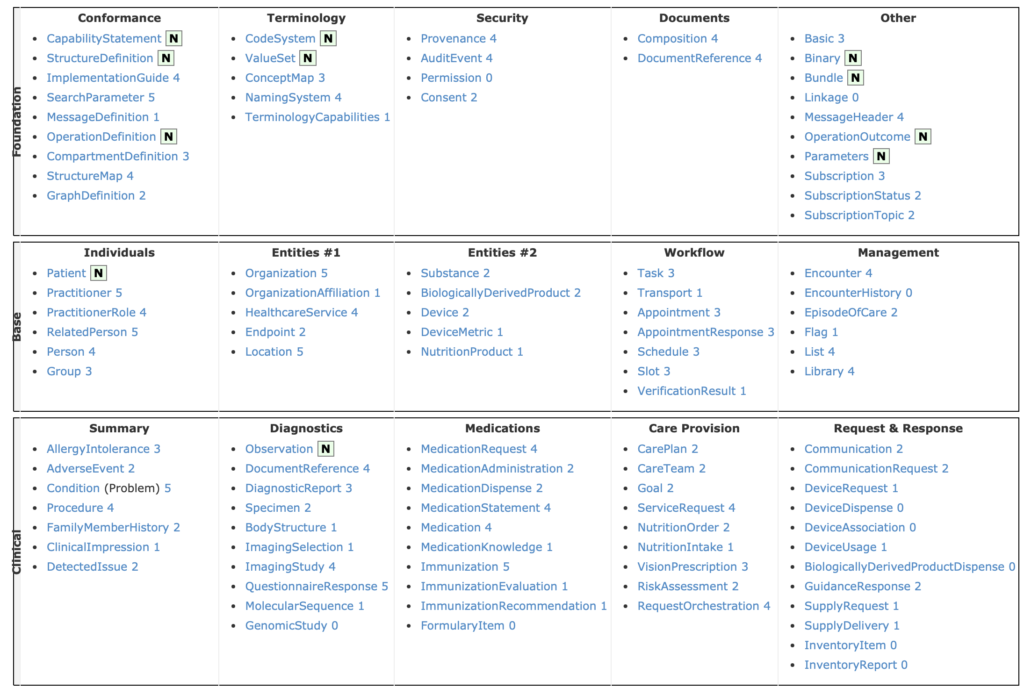
Below is a FHIR resource list structured by type for the latest version of the specification FHIR V5. This comprehensive FHIR resources list includes all base resources as well as commonly used profiles, making it easier for developers to locate the right resources for their implementation.
For example, the HL7 FHIR Patient resource must contain information such as the patient’s name, address, telephone number, allergies, condition etc. The hl7 fhir patient resource definition ensures that all these data elements are standardized, so any FHIR-compliant system can interpret and exchange patient information accurately.
As such, when two FHIR-based systems are exchanging data, they will “know” what each field represents without additional tweaking or a need for data conversion. Data from a laboratory information system (LIS) can be easily integrated with and interpreted by a hospital’s electronic medical records (EMR) system.
The key requirements list for FHIR can be defined as:
- Identical definition and representation, including the names of attributes, types of data, and relations between data arrays
- Standardized FHIR resource types attributes (1+2 = Base FHIR resources, defined by the standard specifications, have a standard list of elements, types, and relations between data arrays.)
- Standard metadata, defining the technical context of each resource: ID, version, profile, text narrative, last updated
- Human-readable format.
The resources and resource elements, along with their naming, data types, and the relationships between them, are all defined by the FHIR standard. Each resource can be represented in different formats such as XML and JSON.
Below we will take a more detailed look at an example of an FHIR Resource – a FHIR Patient resource, and the kind of information about the patient it can provide.
(Disclaimer: all information in the given example is fictitious and does not represent a real person)
{
"resourceType": "Patient",
"id": "870bfc6c-654b-4b29-aac3-3315eed565d6",
"meta": {
"profile": [
"http://hl7.org/fhir/us/core/StructureDefinition/us-core-patient|5.0.1"
]
},
"extension": [
{
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-race",
"extension": [
{
"url": "ombCategory",
"valueCoding": {
"system": "urn:oid:2.16.840.1.113883.6.238",
"code": "2106-3",
"display": "White"
}
}
]
}
],
"identifier": [
{
"use": "usual",
"type": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v2-0203",
"code": "MR",
"display": "Medical Record Number"
}
],
"text": "Medical Record Number"
},
"system": "http://hospital.smarthealthit.org",
"value": "1032702"
}
],
"active": true,
"name": [
{
"family": "Kovach",
"given": [
"Amy",
"V."
],
"suffix": [
"Ms."
],
"period": {
"start": "2020-07-22"
}
}
],
"telecom": [
{
"system": "phone",
"value": "378-354-1234",
"use": "home"
},
{
"system": "email",
"value": "[email protected]"
}
],
"gender": "female",
"birthDate": "1987-02-20",
"address": [
{
"line": [
"183 Mountain View St"
],
"city": "Mounds",
"state": "OK",
"postalCode": "74048",
"country": "US"
}
],
"maritalStatus": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v3-MaritalStatus",
"code": "M",
"display": "Married"
}
],
"text": "Married"
},
"communication": [
{
"language": {
"coding": [
{
"system": "urn:ietf:bcp:47",
"code": "en-US",
"display": "English"
}
],
"text": "English"
}
}
]
}FHIR Resource Structure
A FHIR resource is a structured “container” for one clinical concept, like a Patient, Encounter, Observation, MedicationRequest, or Condition. Each resource is built from elements, and each element has a defined data type and rules. Some elements are simple, like a string, boolean, integer, or dateTime. Others are complex, like HumanName, Address, Identifier, CodeableConcept, or Quantity, which package several related fields together.
Resources also have common backbone elements. Most include an id, metadata, and often narrative text, plus coded fields that use standard terminologies. Many elements can repeat, so a patient can have multiple identifiers or names. Constraints like required fields and allowed repetitions are defined through profiles and implementation guides. That is what keeps two “FHIR Patient” resources from drifting too far apart in how they are populated.
Resource Relationships and References
FHIR is designed as a connected graph, not a flat record. Resources link to each other using Reference. For example, an Observation can reference the Patient it belongs to, the Encounter where it was recorded, and the Practitioner who performed it. This linking is what allows systems to reconstruct a patient timeline across many resource types.
FHIR also supports a few patterns for packaging and embedding related data. Contained resources are resources stored inside another resource, used when the embedded item does not have a stable identity on its own or should not be referenced elsewhere. Bundles are collections of resources sent together, often for exchange and search responses.
A bundle can represent a search result, a transaction, or a batch submission. In practice, bundles help move a complete clinical context in one payload, while references keep the relationships clear and navigable.
FHIR Profiles
Among FHIR components this FHIR standard follows the 80/20 rule. FHIR resources are intended to cover around 80 percent of data elements in the healthcare systems, while the other 20 need to be tweaked to cover specific use cases. This way, FHIR provides both the base and the means to expand that base to suit your needs.
In the FHIR standard, resources are described loosely to allow them to be adapted for a specific context. Extending or constraining elements in the base resource is called profiling. Additionally, FHIR security considerations play a crucial role in ensuring that profiled resources are used safely and in compliance with data protection standards. Hence, a modified FHIR resource is referred to as an FHIR profile. Profiling helps define the missing extensions that should be added and how API functions and terminologies should be used (terminologies in FHIR® are defined using value sets and code systems).
A typical FHIR profile will consist of:
- general requirements describing its goal, category, and the original resource configured by the profile
- a snapshot section with a full configuration of the profiled resource
- a differential section focused on the differences between the profile and the base resource (This section and the FHIR profiler tool help make profile configuration easier for data analysts)
- Slicing, binding, and FHIRPath rules for constraining or extending resources.
FHIR resources, while covering a lot of use cases, are not one-size-fits-all. Profiling is an essential part of the process of FHIR adoption and development. The most commonly used FHIR profiles vary depending on the healthcare organization and the specific use case. However, several profiles are widely adopted and have become industry standards.
One of the most widely used profiles is the US Core Profile, which is used for exchanging patient information between systems in the United States. It includes a set of common data elements that are required to support a variety of use cases, such as electronic health records (EHRs), patient portals, and public health reporting.
Another widely used profile is the Da Vinci profile, which is a set of FHIR resources and profiles that are designed to support the exchange of healthcare information between payers and providers in the US. It includes resources for claims, payments, and patient information.
Read Also: Mapping Healthcare Data to HL7 FHIR Resources
The Care Connect profile is widely used in the UK for the exchange of healthcare information between systems. It includes a set of FHIR resources and profiles that support the exchange of patient information and clinical documents.
The Argonaut profile is another widely adopted FHIR profile that is designed to support the exchange of healthcare information between systems. It is focused on the exchange of patient information and clinical documents and is used in the United States and Canada.
To help business analysts and developers create profiles for their specific context, there are various profile authoring tools. Our team has published a detailed comparison of such tools, where we compare the Kodjin Profile Editor, the Forge from Fire.ly, and Trifolia-on-FHIR.
Below, we’ll take a look at the Carin for Blue Button Patient profile snapshot. The base FHIR Patient resource contains an exhaustive set of data elements, but not all of them are relevant in this particular case. If you take a look at the snapshot provided below, you will notice some elements marked with a red S, those are fields that must be supported in the API to conform to the C4BB Patient resource. Some elements had their cardinality changed to one, meaning this element must appear at least one time.
FHIR Implementation Guide
Implementation guides (IGs) are a collection of FHIR resources (profiles, value sets, examples, documentation, etc.) and rules that are to be used for specific purposes.
IGs describe how FHIR resources are to be used in a particular clinical context and are key to providing a fast and seamless implementation of FHIR. For instance, IGs can describe which patient attributes should be filled in to comply with national standards or which terminologies should be used.
Typically, implementation guides are published online after being created with an FHIR IG publisher. You can find some examples of published IGs on the FHIR registry.
Implementation Guides specify:
- Rules about which resource elements are or are not used, and what additional elements are added that are not part of the base specification
- Rules about which of FHIR’s RESTful API, messaging, and document features are used, and how they are used
- Rules about which terminologies are used in particular elements
- Descriptions of how the Resource elements and API features map to local requirements and/or implementations.
FHIR Data Types
FHIR data types are used to define the resource elements and allow FHIR-based systems to understand what different elements of the FHIR resources represent.
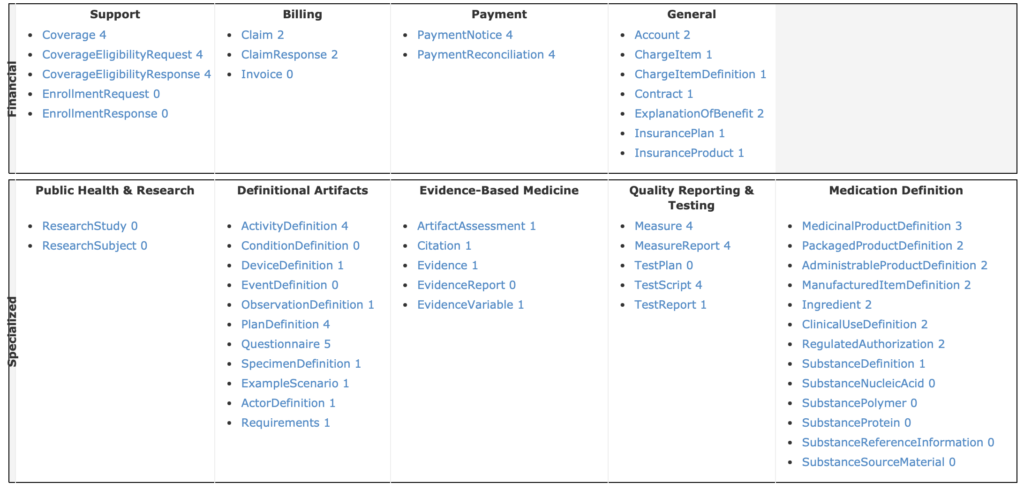
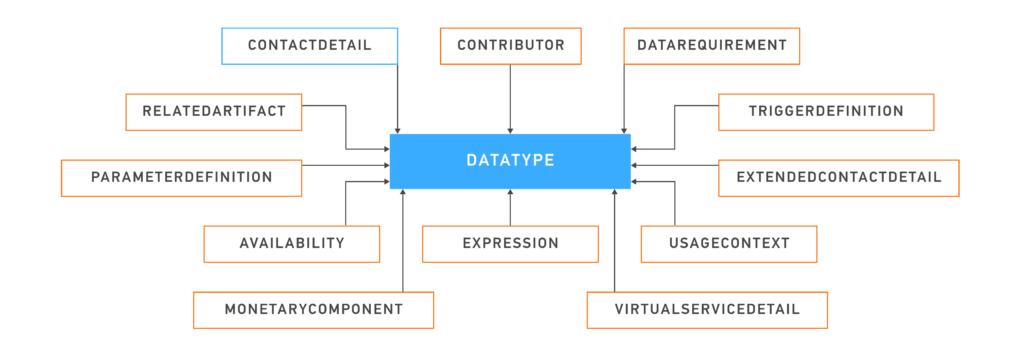
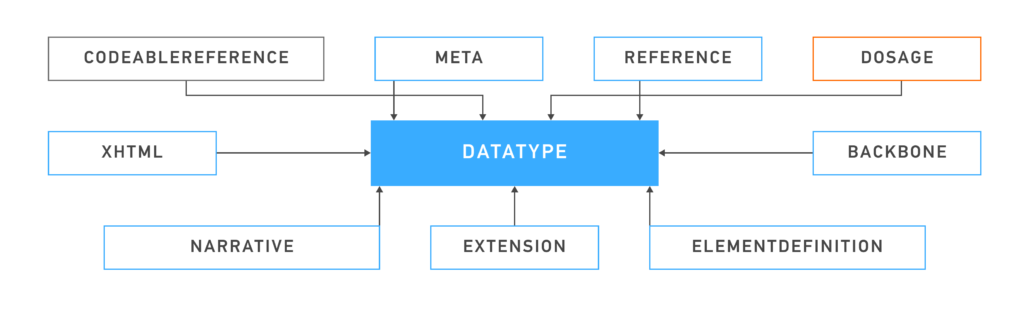
In FHIR, data types are divided into primitive, general-purpose, metadata, and special-purpose data types.
The primitive types of data include string, integer, boolean, etc., each capable of holding a single value.
Below are illustrations that demonstrate the various data types used in the FHIR standard. For more information, you can refer to the FHIR specification page on data types.
Primitive Types
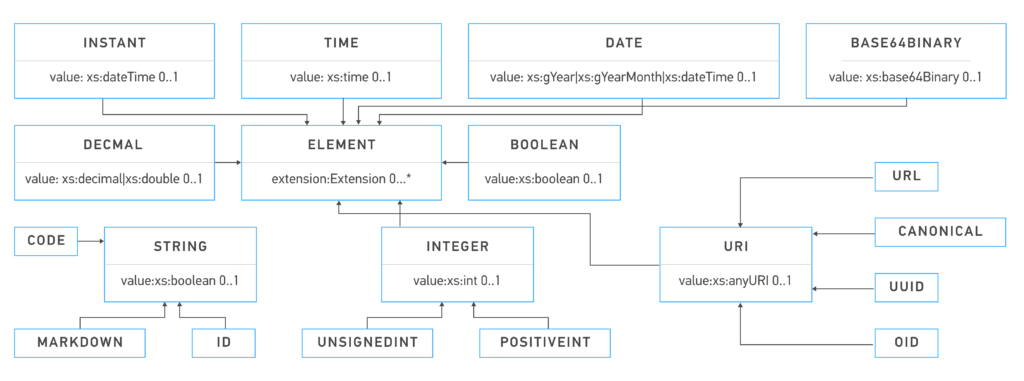
General-Purpose Datatypes
Metadata Types
Special Purpose Datatypes
FHIR REST API
A REST API (also referred to as RESTful API) is an application programming interface (API) that follows the requirements of the REST architectural style and allows for interaction with RESTful web services. The advantages of RESTful architectures include lightweight interfaces, allowing fast transmission and processing of data.
FHIR utilizes REST for data exchange in its API and provides different endpoints for different types of transactions with the resources. The fast FHIR REST API call consists of a request from a client and a response from a server, enabling quick and efficient data sharing. FHIR server testing is essential to ensure these interactions are secure, efficient, and compliant with healthcare standards.
For example, third-party applications, such as a Patient’s Portal app, can request data about the patient from an EHR system through an integrated FHIR API. The request specifies which type of data and how much of it needs to be pulled from the EHR server.
FHIR Validation and Conformance
FHIR validation is how teams confirm a resource is “well-formed” and meets the rules they agreed to follow. In practice, validation usually happens in layers.
First comes syntax and structure. The resource must be valid JSON or XML. Required elements must be present. Data types must match what FHIR expects, like dateTime, CodeableConcept, or Reference.
Next comes profile conformance. Most real projects do not validate only against the base FHIR spec. They validate against a profile from an implementation guide. Profiles tighten the rules by saying which elements are required, what value sets are allowed, and which references are valid. This is where you catch “it is FHIR, but not our FHIR.”
Then comes terminology validation. Codes should come from the right code system and value set. For example, a status field should use the allowed code list. This step prevents quiet inconsistencies that break analytics later.
Finally, many teams add reference and business-rule checks. References may need to resolve to real resources. Some rules are workflow-specific, like “a finalized result must have an effective time.”
Tooling varies, but the idea is the same. You run a validator, you capture clear errors, and you treat failures as fixable events. Many FHIR servers also support an explicit $validate operation, so producers can test payloads before submitting them.
FHIR Maturity and Stability
Not every FHIR resource is equally “ready” for production. HL7 tracks stability in a few ways, and these signals help you choose what to build on.
One is Normative vs Trial Use. Normative content is meant to be stable across releases. Trial Use can still change as the community learns from implementations. Trial Use is not “unsafe,” but it can require more adjustments over time.
Another is the FHIR Maturity Model (FMM) level. It is a scale that reflects how mature a resource is, based on real-world use and review. Higher FMM usually means fewer surprises.
For most production systems, teams start with the resources that have broad adoption and clear patterns. Common “core” choices include Patient, Practitioner, Organization, Encounter, Condition, Observation, DiagnosticReport, Procedure, MedicationRequest, AllergyIntolerance, Immunization, DocumentReference, and Bundle. These cover a lot of daily interoperability needs.
Security and Privacy in FHIR
FHIR as a standard does not inherently provide security features. Its primary focus is on defining the structure for healthcare data and how it can be exchanged. FHIR specification assumes that security will be provided by the underlying system or through other layers of the technology stack. In other words, while FHIR outlines how resources like patient records should be structured and how they can be accessed or modified via APIs, it does not dictate how these operations should be secured.
This approach offers flexibility in implementing security features, allowing organizations to layer their own protocols such as encryption, access control, and auditing on top of FHIR. Many systems use HTTPS for data encryption and OAuth 2.0 for authentication. FHIR often leverages existing security frameworks like SMART on FHIR, which standardizes integration with OAuth 2.0 and OpenID Connect for secure authorization and single sign-on.
Conclusion
The FHIR (Fast Healthcare Interoperability Resources) standard has emerged as a secure framework for achieving true healthcare interoperability for a reason. In this article, you learned how the main components of the FHIR standard are facilitating interoperability around the globe.
Our expertise in creating FHIR facade interfaces ensures streamlined integration of complex healthcare data systems, enhancing the user experience and efficiency.
Next, you can learn more in-depth about the FHIR Standard, FHIR structure components, and resources in our Ultimate Guide – What is FHIR.
Our FHIR development team is always open to cooperation and collaboration to help your healthcare organization achieve a fast and agile data exchange. Contact us to see how we can help with your project!
FAQ
What is the basic building block of FHIR?
FHIR Resources are the basic building blocks of the FHIR specification. They comprise an indivisible unit that contains various clinical data in a structured manner. Each resource is defined by the context of its use. For example, the patient resource contains the most important information about the patient, such as name, address, age, and so on, while Observation resource contains information about vital signs, test results, clinical findings, etc.
How many resources are in FHIR?
In the latest version of FHIR (v. 5), there are 153 resources. The specification remains in active development, and as such, new resources are added continuously.
What is the difference between FHIR and SMART on FHIR?
SMART on FHIR combines FHIR and the SMART platform. Essentially, it’s a set of open standards and specifications that work together to help healthcare developers create and integrate third-party healthcare apps. FHIR standardizes data, while SMART standardizes how this data can be accessed. You can read more about the differences between FHIR and SMART and the technical components for SMART on FHIR on our blog.








