A steady replacement of conventional fee-for-service models with value-based care (VBC) is changing the healthcare scene to give quality priority over volume. This paradigm shift to the value-based care model in healthcare seeks to better clinical outcomes, raise patient satisfaction, and lower the general cost of treatment.
According to a report by Humana, Inc, the members participating in their value-based care program, the Humana Medicare Advantage, had 32.1% fewer inpatient admissions and 11.6% fewer emergency department visits in 2023. Value-based care models also resulted in a 25.8% drop in medical expenses relative to original Medicare, with those savings reinvested into member-focused benefits like cheaper premiums, home care services, prescription delivery, and healthy food vouchers.
This article explores the nuances of value-based care and examines its advantages, comparisons with other models, objections, and potential consequences.
What Is Value-Based Care?
A comprehensive value-based care definition in healthcare is a payment model based on the quality and results of patient treatment instead of service count. This healthcare delivery system redefines the conventional financial incentives that control hospitals, doctors, and other healthcare providers.
In healthcare, value is defined by a patient’s health outcomes improving in relation to the expenses paid for such improvement. Value-based care is essentially about increasing the capacity of the healthcare system to provide patients with more value, with an eye on bettering health outcomes above cost control.
Maria Ansari, MD, CEO, and executive director at The Permanente Medical Group
Under VBC, assessed by patient health outcomes, payment is directly correlated with the treatment quality. This approach of the value-based care model in healthcare differs from the conventional fee-for-service (FFS) system in which clinicians are paid for the number of treatments rendered independent of the outcomes. In the U.S., the Centers for Medicare & Medicaid Services’ (CMS) value-based care programs are designed to incentivize providers to improve care quality and efficiency, aligning payment with better patient health outcomes.
The Core Principles of Value-based Care
Patient-Centric Focus:
VBC positions the patient at the center of the medical process. A deep understanding of patient requirements, preferences, and values is part of this approach. It underscores tailored care plans that meet specific patient needs, guaranteeing treatment is clinically successful and aligned with what patients consider vital.
In value-based care in healthcare, patient engagement and satisfaction are the main indicators. Providers are encouraged to build stronger patient-provider connections, communication, and patient involvement in decision-making over their treatment.
Considering aspects outside acute medical demands, including social determinants of health, emotional well-being, and long-term quality of life, VBC’s patient-centric emphasis also extends to a more comprehensive picture of health.
Quality Over Quantity:
With the VBC approach, the quality of treatment supersedes the count of tests, treatments, or visits. This change forces clinicians to carefully consider the need for and success of every intervention.
In value-based care in hospital settings, there are several quality measures, including the effectiveness of treatment, patient safety, and care coordination. Avoiding needless treatments, lowering mistakes, and preventing hospital readmissions motivates providers.
By emphasizing the delivery of treatment that improves patient health, this idea helps create a more sustainable healthcare system by lowering wasted spending on pointless or duplicated treatments.
Data-Driven Decision Making:
Value-based care relies on strategically applying healthcare data and analytics to improve patient outcomes and optimize processes. Tools for data analytics help companies determine best practices, evaluate performance against benchmarks for quality, and guide patient care decisions grounded on facts. This approach enhances individual patient results and promotes a better understanding of the efficacy of healthcare strategies. Predictive analytics, for example, can help estimate patient demands, enabling proactive interventions to improve the efficiency and quality of treatment.
AI can streamline processes, improve diagnosis accuracy, and adjust treatment strategies. For instance, AI can examine medical images to find irregularities the human eye might overlook, enhancing early diagnosis and treatment results.
VBC models can revolutionize healthcare delivery by using these technologies, highlighting quality and efficiency to improve patient outcomes and lower costs.
Value-based Care Benefits
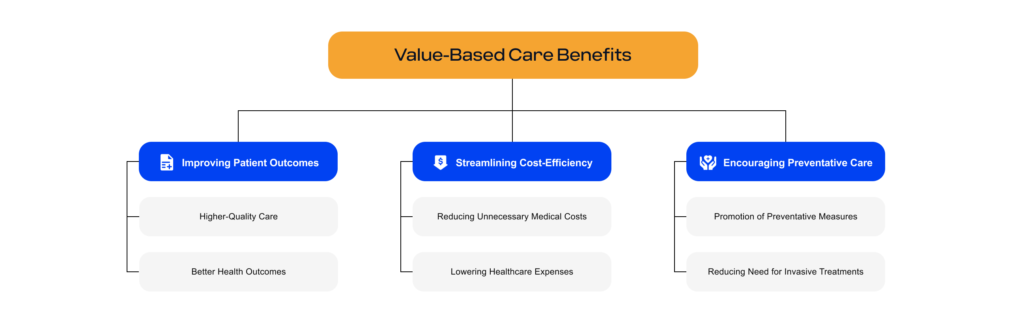
Benefits of value-based care
Improving Patient Outcomes
1. Higher-Quality Care:
- Value-based care (VBC) inevitably creates better quality healthcare services. Focusing on outcomes motivates healthcare professionals to use the best treatment plans and improve their treatments depending on patient responses. This focus results in a more evidence-based approach whereby data and verified findings direct decisions.
- Improving results depends much on improved care coordination under VBC. Because providers are paid for the overall health of their patients, there is more focus on guaranteeing smooth communication and cooperation across different healthcare providers. This all-encompassing strategy reduces treatment gaps, enabling more thorough and continuous healthcare delivery.
2. Better Health Outcomes:
- The outcome-centric nature of VBC means that patient health results are closely monitored and measured. This focus encourages a shift from merely treating symptoms to addressing underlying health conditions and working towards long-term health and wellness.
- Chronic disease management is significantly improved in the VBC model. With consistent monitoring and proactive interventions, conditions such as diabetes, heart disease, and hypertension can be managed more effectively, reducing the likelihood of complications and enhancing the overall quality of life for patients. These improvements represent key value-based care benefits for patients with complex conditions.
Cost Efficiency in Healthcare
1. Reducing Unnecessary Medical Costs:
- Value-based care removes needless tests and procedures, therefore contributing to cost efficiency. Providers are less likely to request unnecessary treatments since payment is not contingent on service volume. Along with lowering immediate expenses, this cut in pointless healthcare treatments reduces the danger of adverse effects or problems from over-treatment.
- Additionally, VBC systems lessen administrative expenses. Lessening the administrative load of handling many claims and coordinating different services allows for more efficient healthcare delivery and lower overhead costs by concentrating on effective treatments and simplifying care operations.
2. Lowering Healthcare Expenses:
- Value-based care models can significantly lower overall healthcare expenses. By improving care coordination and focusing on effective treatments, VBC helps reduce hospital readmissions and emergency room visits, among the most expensive forms of healthcare.
- Preventive care and early intervention, which are emphasized in value-based care in hospital settings, can mitigate the progression of diseases and reduce the need for more complex and costly treatments in the future. This forward-thinking approach improves patient health and contributes to long-term savings in healthcare expenditures.
Encouraging Preventative Care
1. Promotion of Preventative Measures:
- In VBC, there is a strong emphasis on preventive care as a means to improve health outcomes and reduce costs. Providers are motivated to engage patients in routine health screenings, vaccinations, and lifestyle counseling. This proactive approach aims to catch health issues early when they are typically more manageable and less expensive to treat.
- Preventative care in VBC extends beyond clinical settings. It includes community-based interventions and education on healthy living, which is crucial in preventing chronic diseases and maintaining overall well-being.
2. Reducing the Need for Invasive Treatments:
- Maintaining a regular schedule of checkups, effectively managing medications, and making lifestyle changes are common components of VBC practices for chronic illness management. These steps enable efficient control of illnesses, lowering the frequency of cases when surgical or high-risk treatments are required.
- Early identification and consistent monitoring also help VBC-implemented systems lower the risk of conditions developing to the point of requiring costly and intrusive procedures.
Comparing Models: Value-Based Care vs. Fee-for-Service
The conventional way healthcare reimbursement is done is via the fee-for-service (FFS) model. Tests, treatments, and office visits are all considered separate services under this model, and providers get payment for each one. A provider’s compensation is directly proportional to the number of services they deliver; this system is essentially volume-driven.
Because of their simple billing procedures and the obvious transactional link between services provided and payment received, FFS models have long been the standard in healthcare systems worldwide. This straightforwardness has contributed to the long-standing status of FFS as a standard in healthcare financing.
Despite its simplicity, FFS is often criticized for encouraging quantity rather than quality. By incentivizing more procedures and visits, the model can contribute to unnecessary interventions, escalating healthcare costs, and inconsistent patient outcomes. These shortcomings are precisely what the value-based care model aims to address.
Dr. Richard J. Baron, President and CEO of the ABIM and ABIM Foundation, highlights a deeper concern among healthcare practitioners:
“I think fee-for-service has really rotted our brains as practitioners. For example, it might be easy to believe that if a procedure or treatment isn’t on the fee schedule, it must not be valuable. Many of the things we do for patients, including in primary care, may not be represented in a fee-for-service schedule but are nevertheless tremendously important and do, in fact, deliver incredible value.”
This viewpoint highlights the structural flaws in the FFS model that lead to important patient-beneficial activities like care coordination, counseling, and prevention being either undervalued or not included in reimbursement schedules at all, even though they play a crucial role in enhancing health outcomes.
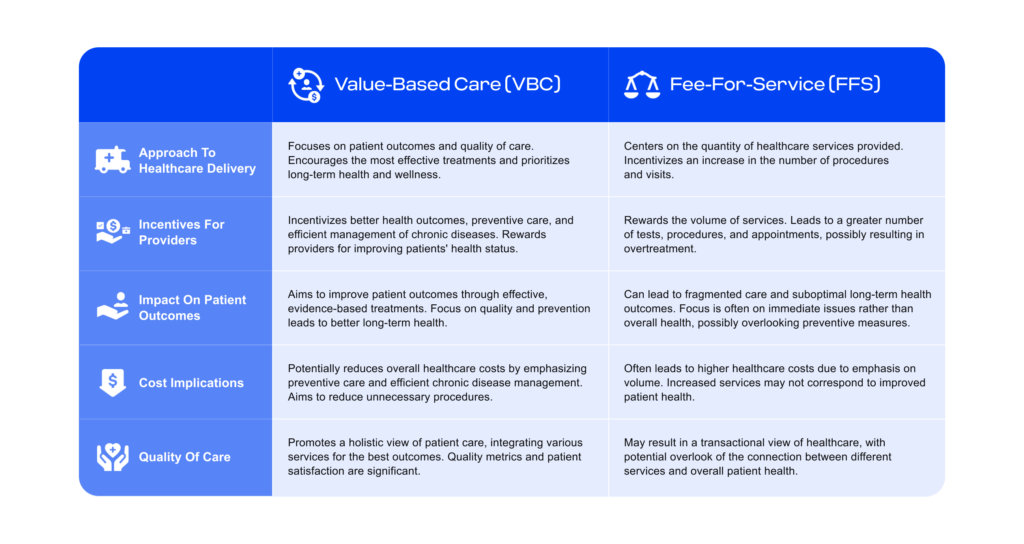
Value-based care vs fee-for-service healthcare models
While the fee-for-service model has been the traditional backbone of healthcare reimbursement, its focus on quantity rather than quality has led to numerous inefficiencies and variable patient outcomes. Value-based care is a promising alternative, prioritizing patient health outcomes and overall care quality, potentially leading to a more sustainable and effective healthcare system.
Criticisms and Challenges of Value-Based Care
Concerns About Quality Metrics
The criteria used to measure care quality are a frequent point of contention when people talk about VBC. Some worry that these measures oversimplify healthcare quality as they don’t always account for the complexities of patient care.
Some worry that if we put too much emphasis on certain measures, we may fail to pay enough attention to aspects of patient care that are harder to measure but just as crucial to their well-being.
Administrative Burdens
Administrative hurdles may arise as a result of VBC models. Diverting focus from patient care to tracking and reporting the many indicators needed for VBC may be time-consuming and resource-intensive.
“Metric fatigue,” in which healthcare practitioners feel overwhelmed by the requirement to continuously measure and report different treatment components, might result from the heightened focus on data reporting and documentation.
Impact on Small Practices
The transition to VBC can be especially tough for smaller firms. Another major obstacle to entrance is the potentially large investment in technology, data analytics, and administrative support that may be necessary.
Some worry that VBC’s requirements and complexity would further erode patient choice and competition in the healthcare industry by eroding the gap between big healthcare systems and smaller, independent practitioners.
The Future of Value-Based Care
Interoperability of Data
Interoperability and healthcare data standards, such as HL7 FHIR, are foundational to the success of value-based care. Although EHRs are useful for preserving patient information, VBC relies on the capacity to aggregate and share this data across different healthcare systems to monitor outcomes and coordinate care effectively. Leveraging FHIR for value-based care is critical, as it enables seamless data exchange, supports care coordination, and enhances the ability to measure and report on quality metrics.
There is a long way to go until we have real patient data exchange, even with sophisticated EHR systems like Epic. To keep up with the requirements of VBC models for data liquidity and interoperability, EHRs must undergo continual evolution. That is why Edenlab is dedicated to offering FHIR-based solutions that connect disparate systems and guarantee the smooth transfer of patient records.
Within the VBC paradigm, healthcare professionals may make data-driven decisions and enhance patient outcomes using interoperability frameworks to get a comprehensive picture of a patient’s health. This picture includes the patient’s current drugs, history of treatments, and comorbidities.
Artificial Intelligence (AI) and Machine Learning
AI and machine learning are revolutionizing VBC by delivering cutting-edge data analysis and decision-making capabilities. These tools can detect patterns in massive datasets, estimate patient risks, and recommend the best treatment options.
AI algorithms may assist in personalizing patient treatment plans, an important part of VBC. They enable healthcare professionals to personalize therapies to unique patient features, enhancing care efficacy and efficiency.
Data Analytics
Advanced data analytics are critical for assessing results and improving care procedures at VBC. They give insights into the most successful therapies, suggest areas for development, and aid in tracking progress toward specific healthcare objectives.
Predictive analytics can help identify patients at risk of acquiring specific disorders, enabling earlier treatments and improved chronic disease management.
Conclusion
Value-based care offers a major shift in healthcare delivery, promising better patient outcomes and cost savings. However, its success is contingent on overcoming implementation obstacles and resolving criticism within the healthcare community. Embracing technology improvements and encouraging collaborative methods will be critical to realizing the full promise of value-based care in healthcare.
FAQs
What is an example of a value-based approach?
An illustration of a value-driven strategy is Accountable Care Organizations (ACOs). This model involves collaboration among hospitals, physicians, and other healthcare providers to ensure the delivery of coordinated, high-quality care for Medicare patients.
Providers are motivated to achieve quality and performance standards—like decreasing hospital readmissions or enhancing chronic disease results—while minimizing overall expenses. When successful, providers benefit from the financial efficiencies achieved through delivering more effective care and aligning clinical and financial goals to prioritize patient value rather than just the quantity of services provided.
What are the six components of value-based care?
The six core components of value-based care include:
- Care coordination – Facilitating smooth transitions across providers and care settings.
- Patient-centered care – Focusing on individual patient needs, engagement, and preferences.
- Evidence-based practices – Applying standardized, proven clinical guidelines to ensure quality care.
- Performance measurement and reporting – Tracking and reporting outcomes, quality, and operational efficiency.
- Population health management – Managing the health of patient populations, emphasizing prevention and chronic disease control.
- Aligned payment models – Using payment structures like shared savings, bundled payments, or capitation to reward value over volume.
How are providers paid in value-based care?
In value-based care, providers are compensated based on the quality and efficiency of care rather than the quantity of services. Payment models include:
- Shared savings programs – Providers share cost savings achieved through better care management.
- Bundled payments – A single, predetermined payment covers all services for a specific treatment or care episode.
- Capitation – Providers receive a fixed per-member, per-month payment regardless of the number of services provided.
Is value-based care more expensive?
While value-based care aims to reduce long-term healthcare costs by emphasizing prevention, care coordination, and chronic disease management, the transition can involve significant upfront expenses. Investments are often needed in areas such as:
- Health IT systems (e.g., electronic health records and data analytics)
- Care management and coordination teams
- Quality improvement initiatives
Although initial implementation costs may be higher, value-based care seeks to generate savings over time by reducing unnecessary services and improving overall patient health outcomes.







