The lack of interoperability in healthcare has posed an obstacle to quality patient care for decades. Interoperability in healthcare is the ability to exchange and use data within different healthcare IT systems and applications. Accessing healthcare data at the right time will help make decisions faster and facilitate efficient care for patients.
The industry requires specific rules for coding and messaging to ensure all healthcare information is readable and accessible by real-time APIs. The history of health data standardization in healthcare within the United States is a vivid example of how public APIs can transform healthcare.
The Importance of Healthcare Data Standards
Leveraging data management and transmission standards is a significant step towards enhancing the healthcare landscape while improving patient access, interoperability, and innovation within the healthcare systems. Here are the key benefits:
Enhanced Patient Access
Allowing patients to access and exchange their data empowers them to take more active roles in healthcare decisions. Modern healthcare data standards are dedicated to allowing patients to securely access structured electronic health information through smartphone applications for the best convenience.
Increased Innovation
By agreeing on common rules and standards, the healthcare industry fosters an ecosystem that is friendly to new applications and other solutions, providing patients and healthcare stakeholders with a broader range of choices in managing the data.
Data Security
Protecting sensitive data is possible by setting strict rules and severe penalties for noncompliance. Standards for ensuring security of health information include mandatory requirements for caregivers, insurers, and other healthcare stakeholders so they could establish a robust mechanism of accessing and exchanging sensitive patient data.
Information Blocking Prevention
Standardization of data exchange and management procedures can help shift from discouraging practices that hinder the exchange of health information among healthcare stakeholders to those that promote data sharing and collaboration, ultimately improving patient care.
The importance of data standardization in healthcare lays in its role in ensuring that stakeholders prioritize patient access, interoperability, and innovation in healthcare. Regulations benefit patients, healthcare providers, technology developers, and other stakeholders by fostering a more connected ecosystem.
Today, we will introduce you to the most prevalent healthcare data standards in the US and describe how they lead healthcare stakeholders to meaningful use of healthcare data.
How Healthcare Data Standards are Developed
Healthcare standards development process can vary depending on a standard development organization and a country. For example, the Office of the National Coordinator for Health Information Technologies in the U.S. defines such stages of standard development as:
- Defining business needs
- Gathering stakeholders for developing a standard’s draft
- The first balloting
- Piloting
- The second balloring
- Maintenance
What are The Standards Used in Healthcare?
According to HIMSS, over 40 standards development organizations (SDOs) aim to address adopters’ needs. Standards developed under these SDOs can be grouped into four main categories:
- Healthcare data exchange standards
- Data privacy and security standards
- Terminology standards
- Content standards
ICD – International Classification of Diseases
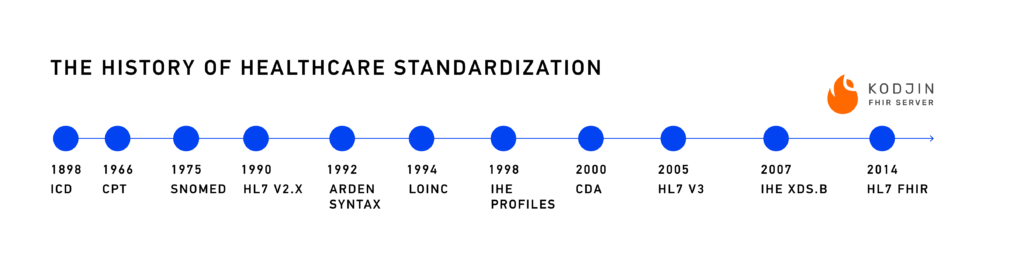
The history of healthcare data standardization can be traced to the end of the 19th century when the International Statistical Institute suggested categorizing causes of death. The first version of the ICD was called the International List of Causes of Death and consisted of 38 categories.
Over the years, this list has transformed into 55,000 codes covering a variety of health conditions. ICD is the first widely adopted standard for health information coding. This standard considerably improved the consistency of health information.
CPT – Current Procedural Terminology
The following important standard was published in 1966 by the American Medical Association. The CPT standard represents a set of codes for standardizing billing and reporting procedures in healthcare (e.g., medical, surgical, and diagnostic procedures). Thanks to this standard, more stakeholders can understand healthcare procedures and analyze their costs and outcomes.
SNOMED CT – Systematized Nomenclature of Medicine – Clinical Terms
SNOMED CT is one of the most widely adopted standards for healthcare data. It is used by healthcare organizations worldwide. SNOMED CT provides standardized medical terminology. Its development started in the 1960s and resulted in an officially launched terminology standard in 2007. SNOMED CT describes all things medicine, which improves the accuracy and consistency of healthcare data.
HL7 V2.x – Health Level Seven Version 2.x
HL7 version 2.0 was published in 1989 and appeared as the first healthcare data standard that defined the format for exchanging healthcare information between systems. The HL7 V2 was more scalable than previous data standards in healthcare. This standard allows transmitting HL7 messages between systems and targets more complex data exchange needs. The wide adoption of this standard has exposed problematic areas of healthcare data exchange and has advanced society toward achieving global healthcare data interoperability.
Arden Syntax
The Arden Syntax is a standardized representation of clinical knowledge in a computer-readable format. This standard has helped spread clinical knowledge across many healthcare organizations. The wide adoption of this standard has greatly improved decision-making within healthcare, for instance, by providing essential alerts such as preventive care reminders, chronic conditions, and drug interaction alerts.
LOINC – Logical Observation Identifiers Names and Codes
LOINC is a standardized database of identifiers, names, and codes for health measurements, observations, and documents. The main goal of the LOINC standard is to provide caregivers with a standard code system for the correct interpretation of observations, lab results, and other information relevant to the healthcare process.
HE – Integrating the Healthcare Enterprise
The IHE profile is the first initiative to provide access to healthcare information for both healthcare providers and patients. IHE profiles define how healthcare actors use standards for addressing use cases. It is based on existing data exchange standards in healthcare, such as HL7 V2. Suppliers of medical equipment and software systems integrate their products with IHE profiles to ensure the meaningful exchange of healthcare information.
CDA – Clinical Document Architecture
CDA is a standard for the electronic exchange of patient information. The HL7 organization developed CDA to provide a standardized framework for exchanging clinical documents in machine-computable and human-readable ways. CDA sets up rules for organizing patient data (demographics, patient history, lab test results, etc.). CDA has leveraged innovations from the third version of HL7 standards.
HL7 V3 – Health Level Seven Version 3
The HL7 V3 standard was developed in response to accommodated healthcare data exchange challenges, specifically interoperability ones, to establish a smooth exchange between systems and applications. The standard is based on specific data models, also known as RIM, exchanged via messages in XML format. RIM stands for Reference Information Model, which was meant as a solution for achieving the highest healthcare data interoperability level.
In our previous article on semantic interoperability, we described the peculiarities of RIM and the reasons why the HL7 V3 standard had not been widely recognized.
IHE XDS.b – Cross-Enterprise Document Sharing, Basic
The IHE XDS.b standard was launched to improve data exchange between enterprises by providing prescriptive profiles and standards-based data-sharing specifications to help share EHRs, reports, clinical documents, and other information more easily.
It is a partial list of examples of standards in healthcare developed in the US to cover data representation, exchange, and storage issues. There are other fundamental healthcare standards, which provides a global common language for health terms, or X12: the standard that defines the format, structure, and content of administrative and financial transactions between healthcare organizations.
It is crucial to ensure the proper realization of all healthcare data standards by regulations. FHIR targets this problem with Implementation Guides (IGs). IGs developed by healthcare stakeholders and FHIR accelerators like Da Vinci and CARIN provide a standardized set of healthcare data elements and exchange protocols.
FHIR Implementation Guides solve data standards realization issues and keep up with modern data exchange and storage practices.
The deep analysis of healthcare gaps made the US government and industry stakeholders understand the need to leverage the FHIR standard. Unfortunately, the high cost and complexity of HL7 V3 standard integration have ended the attempt to achieve global interoperability in healthcare.
Specifying the most problematic aspects of healthcare data exchange helped stakeholders overcome data exchange barriers.
Read also: TEFCA in Healthcare
Modern Healthcare Data Exchange Barriers
According to JASON Report Task Force Final Report, the list of data interoperability challenges in healthcare featured:
- Complicated clinical care and research processes due to the absence of meaningful interoperability in the US (lack of standardized data structure, poor data security measures, limited data control for patients, and resistance to leveraging new technologies and standards within healthcare organizations).
- Lack of justification for the replacement of existing clinical and financial systems (approach implied by the HL7 V3 integration).
- Lack of an adequate timeline for leveraging changes in the current interoperability paradigm.
The Report included several recommendations for targeting the above-mentioned problems.
1. Join industry forces and the Government to define a market-based exchange architecture based on a loosely coupled, coordinated architecture for exchanging data via a public API, a standard data sharing arrangement, and standard-based data services for the API’s realization.
2. Focus on data exchange and consumer access use cases.
3. Specify minimum data elements, formats, and document types for support by public APIs.
4. Ensure simplified patient access and control over healthcare data via a tethered portal by leveraging OAuth 2.
5. Define FHIR as a technical standard to achieve meaningful use of healthcare data through the use of Public APIs.
FHIR for Addressing Data Exchange Challenges
The Final Report prescribed leveraging modern FHIR and SMART on FHIR standards as a foundation for building public APIs.
Why is FHIR considered to be the base standard for building public APIs?
Public API is a main component of the FHIR standard. The FHIR Application Programming Interface is a standard specification that describes how to use common technologies for smooth healthcare data exchange. Public API is the most straightforward tool for manipulating and retrieving data from one system to another. Therefore, FHIR APIs are based on REST architecture.
REST stands for Representational State Transfer and is the most widely used data exchange method. RESTful APIs exchange data using HTTP, the fundamental protocol for data exchange on the internet. FHIR APIs successfully communicate with FHIR-first servers and interact with FHIR resources with CRUD commands. A successful FHIR server implementation ensures seamless interoperability between systems and supports efficient data exchange workflows.
However, REST architecture doesn’t cover the authorization and authentication processes, which are essential to define since it allows actors to access health data via third-party applications. Therefore, ensuring a smooth and straightforward authorization process is necessary for providing patients with access and the ability to control their data.
SMART on FHIR: The Out-Of-The-Box Solution
Our previous article about SMART on FHIR described how its architecture works and how it encourages developers to create new healthcare IT solutions. You will find a detailed scheme of the SMART on FHIR authorization and authentication processes there.
Like RESTful, SMART is a standard-based API based on the OAuth 2.0 standard. SMART defines protocols for accessing EHRs and simplifies the development of new applications by excluding the need to build an EHR connection database from scratch.
The SMART platform offers a free sandbox for effective testing and deployment of new applications. SMART has migrated from the list of JASON’s recommendations into the standards-based API certification criterion of ONC’s 21st Century Cures Act Final Rule.
The SMART platform is based on FHIR resources. It provides developers with a comprehensive toolset for building plug-and-play applications to access EHRs, which includes protocols for authentication, authorization, and user interface integration. SMART on FHIR enables streamlined access to health data and ensures its meaningful use.
Kodjin: Ensure Health IT Compliance
Leveraging the SMART on FHIR interface is crucial for entering the health IT market. Our developers are avare of all ONC certification requirements and will make your project compliant with SMART on the FHIR framework and define steps to enter the healthcare ecosystem with a fully interoperable IT solution.
Check out the national eHealth system development project details to discover how to transform legacy systems with the FHIR facade and other top-notch enterprise-level tools. For more information about FHIR, read our FHIR overview.
FAQs
What is the connection between data standards and healthcare?
Healthcare and data standards are directly connected since the latter ensure consistency of data collecting, storing, and exchanging within healthcare.
Why are data standards important in healthcare?
The importance of standards in healthcare is undisputed since it provides a standardized way to simplify workflows and achieve interoperability in healthcare.
What are the benefits of healthcare data standards?
The value of healthcare data standards has numerous benefits, including improved data quality and streamlined data exchange, allowing access to needed data in time and improving patient outcomes.
Why is the digital exchange of structured data called electronic data interchange?
The digital exchange of structured data between organizations is commonly called electronic data interchange (EDI), not simply “electronic data.” EDI refers to the computer‑to‑computer interchange of standardized data formats, such as purchase orders or invoices, using agreed message standards. It enables automated transfer of structured information without manual intervention.
What is clinical data standardization?
Clinical data standards ensure that healthcare information is stored and communicated with unambiguous meaning. Standardized data supports clinical practice, analytics, and research, while enabling interoperability between disparate health‑IT systems. Examples include HL7 V2/V3, FHIR, DICOM, SNOMED CT, and ASC X12; these standards promote consistent structure and terminology across clinical data.
What is healthcare data normalization?
Data normalization organizes heterogeneous health information into a common structure and vocabulary. It starts by collecting patient records from EHRs, lab systems, billing, and insurance databases and integrating them into a centralized repository. Standardizing and semantically translating these records creates a unified dataset that supports future queries, advanced analytics, and informed decision‑making.





