HL7 and EMR/EHR interoperability are essential in today’s healthcare. Achieving seamless EHR interoperability often requires efficient FHIR Data Mapping, ensuring that healthcare data is accurately translated between systems. All healthcare stakeholders try to find the best ways to secure, exchange, and access health data without obstacles. That’s why the importance of interoperability EHR is increasing nowadays.
For example, in the US, the Office of the National Coordinator for Health Information Technologies (ONC) noted increased electronic health records (EHR) use, which allows access to critical health data. However, the mechanism of health data integration from various providers needed some advancement and standardization to ensure EHR interoperability.
For our partners at Elation Health, we have created a solution to ensure interoperability of their EHR platform while meeting the compliance standards of the ONC’s 21st Century Cures Act, particularly the HL7 FHIR standard.
The Health Level Seven (HL7) is the ANSI-certified organization that develops health data standards and makes tremendous efforts toward gathering and assisting healthcare stakeholders to create interoperable EHR solutions.
The HL7, along with other international standardization groups (such as ISO, CEN, ASTM, and others), have greatly contributed to EHR interoperability, which we are going to talk about in this article.
What is EHR interoperability?
The definition of EHR/EMR interoperability involves the capability of various electronic health record (EHR) systems to enable healthcare providers to seamlessly access and share patient data. This ensures that the meaning of the information exchanged is preserved and that there is timely access to the data within an EHR system.
Levels of EHR interoperability
Electronic health records interoperability has three levels, each serving a distinct purpose in facilitating seamless communication between systems and applications.
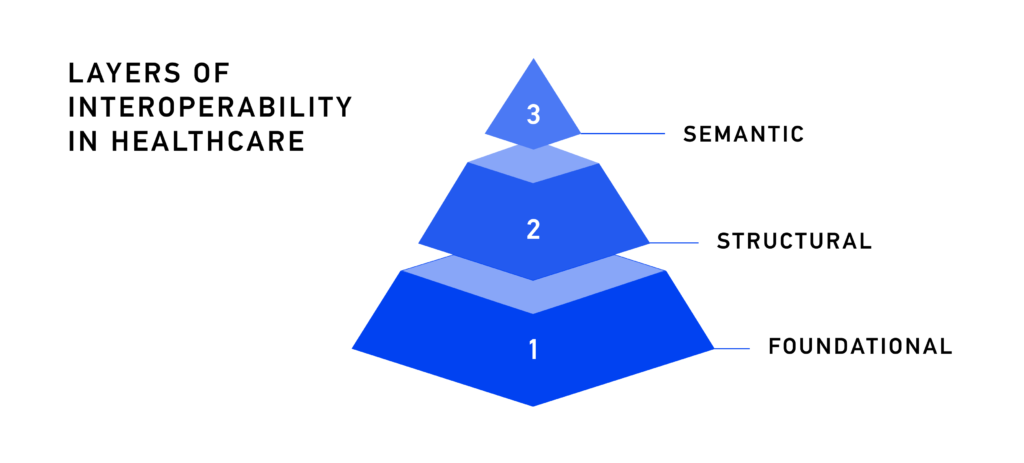
• Foundational Interoperability refers to the ability to transfer raw data from one system to another efficiently and securely. This level of Interoperability is typically achieved through the use of data transmission standards without addressing the interpretation of the exchanged data.
• Structural Interoperability can be built upon foundational Interoperability for defining the format and organization of exchanged data. Achieving this level requires arranging data fields and the coding schemes used for the data exchange through leveraging messaging standards.
• Semantic Interoperability is the highest level of Interoperability that allows for exchanging data in a meaningful way, so data is not only understood but also interpreted by receiving systems in a meaningful way. Ensuring semantic Interoperability requires standardized terminology, vocabularies, and ontologies.
Benefits of EHR Interoperability
According to Statista, the global electronic health records (EHR) market value is forecasted to grow from 29 billion U.S. dollars in 2020 to 47 billion U.S. dollars in 2027.
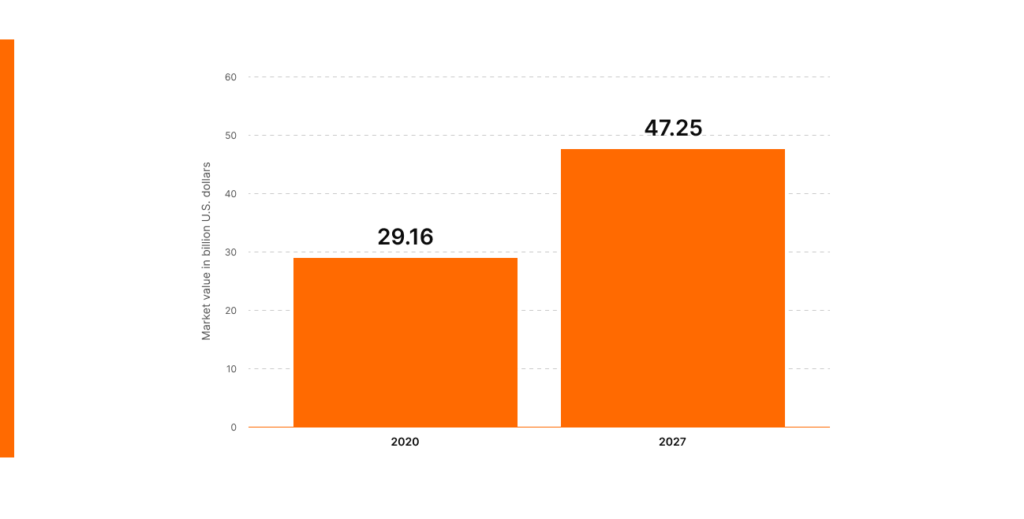
This level of growth is easily explained since EHR allows exchanging health data in real-time, which helps reduce healthcare costs and contributes to patients’ safety.
The Office of The National Coordinator for Health Information Technology (ONC) mentions the following benefits of EHR interoperability:
- Enables better workflows.
- Reduces ambiguity.
- Facilitates data transfer among EHR systems.
- Enhances communication among healthcare stakeholders.
- Improves the delivery of healthcare.
- Ensures the availability of the right data at the right time to the right people.
Electronic health records (EHRs) do the aforementioned tasks and enhance communication between all healthcare providers. The EMR works within healthcare organizations. The EHR allows clinicians to go beyond and share lab results, medical notes, and information from other establishments involved in the healthcare of a specific patient.
Interoperability of electronic health records is the ability to exchange medical records between different providers or systems. Integration of electronic health records contributes to the creation of an interoperable environment. The ONC names four key technology areas for integration with EHR to achieve complete EHR interoperability:
- Application interaction with users
- System communication
- Information processing and management
- Consumer device integration
There are a lot of benefits of EHR interoperability for businesses, such as:
- Streamlined workflow: reduces paperwork and work time by providing actual care, managing appointments, and minimizing latency in health care.
- Reduced administrative costs: eliminates the need for physical chart storage and data transcriptions. It significantly reduces the time needed for communication between hospitals, labs, pharmacies, and other participants in the healthcare process.
Read Also: Pharmacy Data Interoperability
Why is HL7 important to the EHR?
For over 30 years, HL7 V2 messages have been used as the primary method to achieve HL7 EHR interoperability. Since then, new interoperability solutions have been developed to replace outdated HL7 message types with modern solutions like FHIR, which has brought healthcare interoperability to a whole new level.
However, manufacturers of medical systems are not quite there yet with technologies for integrating medical hardware with FHIR solutions. HL7 V2 messages remain the most widely used and recommended for data exchange between laboratory systems and other medical equipment.
HL7 V2 Messages
Messages allow the transfer of data between LIMS (Laboratory Information Management System), EHRs, financial, and other systems. The Health Level 7 messaging standard facilitates data transfer across disparate systems. HL7 messages allow for healthcare interoperability and define the format for health data sharing.
Types of messages:
- ACK- General Acknowledgment – an ADC message is sent by message receiving system back to the sending interface to identify a message as received.
Example:
MSH|^~\&|LABADT|DH|EPICADT|DH|201301011228||ACK^A01^ACK
|HL7ACK00001|P|2.3
MSA|AA|HL7MSG00001- ADT- Admit, Discharge, Transfer – provides information about trigger events and the demographic information of a patient.
Example:
MSH|^~\&|EPIC|EPICADT|SMS|SMSADT|202211031408|CHARRIS|ADT^A04|181
7457|D|2.5| EVN||202211030800||||202211030800 PID||0493575^^^2^ID 1|454721||DOE^JOHN^^^^|DOE^JOHN^^^^|19480203|M||B|254 MYSTREET AVE^^MYTOWN^OH^44123^USA||(216)123-4567|||M|NON|400003403~1129086| NK1||ROE^MARIE^^^^|SPO||(216)123-4567||EC|||||||||||||||||||||||||
|| PV1||O|168 ~219~C~PMA^^^^^^^^^||||277^ALLEN MYLASTNAME^BONNIE^^^^|||||||||| ||2688684|||||||||||||||||||||||||202211031408||||||002376853- ORU – Observation Result – contains information about a patient’s observations and results. Allows transmission of observation results data from the producing system to the ordering one.
Example:
MSH|^~\&|MESA_RPT_MGR|EAST_RADIOLOGY|iFW|XYZ|||ORU^R01|MESA3b|
P|2.4||||||||
PID|||CR3^^^ADT1||CRTHREE^PAUL|||||||||||||PatientAcct||||||||||||
PV1||1|CE||||12345^SMITH^BARON^H|||||||||||
OBR|||||||20010501141500.0000||||||||||||||||||F||||||||||||||||||
OBX|1|HD|SR Instance UID||1.113654.1.2001.30.2.1||||||F||||||
OBX|2|TX|SR Text||Radiology Report History Cough Findings PA evaluation of the chest demonstrates the lungs to be expanded and clear. Conclusions Normal PA chest x-ray.||||||F||||||
CTI|study1|^1|^10_EP1- ORM – Order for treatment or pharmacy – used to transfer information about an order.
Example:
MSH|^~\&|EPIC|EPIC|||20140418173314|1148|ORM^O01|497|D|2.3||
PID|1||20891312^^^^EPI||APPLESEED^JOHN^A^^MR.^||19661201|M||AfrAm|505
S. HAMILTON AVE^^MADISON^WI^53505^US^^^DN |DN|(608)123-4567|(608)123-5678||S|| 11480003|123-45-7890||||^^^WI^^
PD1|||FACILITY(EAST)^^12345|1173^MATTHEWS^JAMES^A^^^
PV1|||^^^CARE HEALTH SYSTEMS^^^^^||| |1173^MATTHEWS^JAMES^A^^^||||||||||||610613||||||||||||||||||||||||
||||||||V
ORC|NW|987654^EPIC|76543^EPC||Final||^^^20140418170014^^^^||2014041817
3314|1148^PATTERSON^JAMES^^^^||1173^MATTHEWS^JAMES^A^^^|1133^^^222^^^^^|(618)222-1122||
OBR|1|363463^EPC|1858^EPC|73610^X-RAY ANKLE 3+ VW^^^X-RAY ANKLE ||||||||||||1173^MATTHEWS^JAMES^A^^^|(608)258-
8866||||||||Final||^^^20140418170014^^^^|||||6064^MANSFIELD^JEREMY^^^^||1148010^1A^EAST^X-RAY^^^|^|
DG1||I10|S82^ANKLE FRACTURE^I10|ANKLE FRACTURE||The HL7 interface allows healthcare organizations to access and retrieve needed data from various systems. HL7 messages improve workflow and interoperability.
Major EHR Interoperability Challenges
1. Patient ID synchronization
Interoperability issues in EHR constitute a significant obstacle to achieving data interoperability in healthcare. Interoperability of data means that a system that receives a message knows how to interpret data on a system level. The programming code should understand a message’s contents to decrypt message data correctly.
The system that receives the data must not duplicate it and must reproduce the data as it is in the system sending the message. This process requires a set of synchronizations to match patients. The scheme below contains a cycle of patient information exchange between two medical systems in different systems using the MPI (Master Patient Index) database.

The Master Patient Index system guarantees patients’ ID authenticity. If MPI defines a patient as a new one, the system creates a new patient. When a system receives a message containing data about the patient that already exists, MPI recognizes it, and the system adds information to an existing patient.
2. DICOM and HL7 interoperability problems
DICOM Digital Imaging and Communications in Medicine is a standard that defines file types for medical images. Thanks to DICOM, physicians can access reports and images. DICOM is a data storage and exchange standard. However, not all systems support the DICOM data transmission protocol. That is why users need a way to transfer DICOM data via the HL7 format.
Architecture of DICOM Network Protocol
Network ⇒ TCP/IP ⇒ DICOM ULP for TCP/IP ⇒ UL Service boundary ⇒ DICOM Message Exchange ⇒ Medical Imaging ApplicationDICOM uses TCP — Transmission Control Protocol. It is a low-level protocol that requires specific technical skills and a deep understanding of network levels and data structure. The problem is that DICOM and HL7 standards are incompatible in a direct way, which complicates the transfer of data between medical equipment in EHR.
HL7 and DICOM standards are crucial for the diagnosis process, which is why enhancement of a time-consuming transmission protocol was required. Leveraging modern electronic health records interoperability solutions can help achieve complete interoperability of HL7 and DICOM formats. RESTful API considerably simplifies the use of TCP. REST APIs are scalable and widely used. They add much-needed flexibility, provide quick and secure data exchange, and ensure DICOM, HL7, and EMR interoperability.
3. HL7 EMR/EHR interoperability
It is difficult to achieve interoperability of HL7 and EHR/EMR systems due to the difference in coding languages, data formats, vocabulary, and system interfaces. For example, the exchange of HL7 CDA (Clinical Document Architecture) requires shared terminologies for the interoperability of HL7 and EHR.
The difficulties mentioned above are only a part of interoperability and HL7 EMR integration problems that must be comprehensively addressed. Global integration of EHR systems ensures quick access to quality care for patients and automated workflow for clinicians. FHIR is the solution to healthcare interoperability problems.
HL7 FHIR Interoperability with EHR
The ONC’s Cures Act Final Rule declares the compulsory adoption of standardized application programming interfaces (FHIR APIs) for a reason. FHIR HL7 EMR integration is an out-of-the-box solution for EHR interoperability challenges discussed earlier.
Moreover, the format of local EHRs and EMRs is no longer an obstacle to achieving interoperability since FHIR provides a standardized way to represent and exchange health data. Using FHIR APIs within EHRs is the key to FHIR HL7 interoperability integration.
FHIR allows for joining data from distinctive EHR and EMR systems. It breaks the exchangeable units into small pieces — FHIR resources. FHIR resources include basic information with a common definition, representation, a set of metadata, and human-readable parts.
FHIR provides flexibility to the healthcare data exchange process and guarantees the correct interpretation of data regardless of differences in various EHRs’ data storage and representation methods.
Why should you set your project on FHIR?
- FHIR is up-to-date – FHIR is the most modern option among all HL7 standards for interoperability. It is the implementers-focused standard that implies existing web technologies, such as XML, JSON, HTTP, and OAuth, which simplifies the creation of new healthcare IT solutions.
- Easy to implement – even coded elements of FHIR resources are human-readable. It has an easy-to-use interface, which ensures speedy integration of EHR interoperability solutions.
- Provides flexibility – resources in the core specification of the standards cover about 80% of common healthcare use cases. FHIR allows for adjusting and combining basic FHIR resources for another 20% of contexts of use.
The FHIR standard is based on a thoughtful analysis of previous HL7 interoperability standards. The interoperability of HL7 and EMR/EHR systems ensures meaningful use of health data and guarantees that data exchange contributes to the quality of care.
Want to know more about FHIR? Check out our ULTIMATE FHIR GUIDE — a must-read material that reveals the history behind the FHIR standard development and how to address healthcare data management challenges with FHIR.
How to Improve EHR Interoperability
Electronic health records interoperability allows providers to access and exchange patient information and improve patient outcomes by avoiding errors and delays. Therefore, enhancing the interoperability of EHR systems is essential for better clinical decision-making and lower healthcare costs.
- Invest in EHR interoperability solutions: Leveraging modern web technologies and using data mapping tools can help improve health data exchange between different systems.
- Follow industry standards: Industry standards such as HL7 FHIR are widely used and can help facilitate data exchange between systems.
- Collaborate with healthcare stakeholders: Collaboration between healthcare organizations can help improve EHR Interoperability. Sharing best practices can help overcome the technical and organizational challenges associated with interoperability.
How to Measure EHR Interoperability
Measuring interoperability helps to ensure that healthcare systems and technologies can exchange data accurately and efficiently. Basic transactions are one of the most critical interoperability aspects for measuring. Consider measuring the volume and type of transactions to exchange information that the receiving system can natively use.
Another factor is the partners and stakeholders involved in the exchange of information. The measurement should be done between patients, providers, payers, and other authorized entities, as well as on a population level, such as registries and reporting.
Measuring standards used in transactions allow tracking transactions are defined by profiles such as IHE, implementation guides, test venues. The procedure should capture message types and standards such as HL7 V2, V3, FHIR®, DICOM, SNOMED CT and LOINC.
User characteristics such as bed size, number of registered network users, and rural or urban locations also play a crucial role in measuring interoperable transactions.
The timing of transactions, whether they are sent in real-time, delayed, or batched later, should also be considered.
The volume of transactions for each technology type and network-reported trend data, such as significant increases or decreases, also needs to be monitored.
Finally, plans to expand on types of transactions a healthcare setting plans to support should be considered when measuring EHR interoperability.
Real-World Examples of EHR Interoperability
Thanks to the creation of the national eHealth system in Ukraine, the country achieved comprehensive management for 36,5 million accounts and the successful integration of 33 Regional EHRs.
- eHealth System: The eHealth system guarantees high-quality, secure data with digital signatures and blockchain-like safeguards.
- Overcoming Challenges: Modernizing an outdated system, Ukraine faced hurdles like outdated registries, low GP computer literacy, and private EHRs.
- Three-Step Transformation: Steps included connecting medical systems, adding secondary/tertiary care, and launching patient cabinets.
- Key Success Factors: Interoperability, HL7 FHIR standards, ICPC-2 methodology, blockchain, ML, and secure access drove success.
Ukraine’s eHealth system is one of the biggest HL7 FHIR projects in the world that showcases the power of EMR/EHR interoperability.
Many healthcare providers have implemented HL7 Integration to facilitate real-time data sharing, making it easier to access comprehensive patient records across various platforms.
Kodjin is Ready to Become Your Reliable Partner
We provide FHIR-based healthcare data management solutions for national-level projects.
Explore details of the National E-Health system project to find out how to improve an outdated system, create a scalable health data repository, and establish a seamless data exchange with FHIR.
Our specialists have a deep understanding of the FHIR integration process. They will help you address healthcare data interoperability challenges, customize the FHIR server for a specific business context, and set your project on FHIR as quickly and efficiently as possible.
FAQ
What is the HL7 EHR interoperability model?
It refers to a set of requirements for interpreting healthcare data by third-party systems with the preservation of the meaning laid in the exchanged information by the system that spawned the data (e.g., compare values from code systems).
What is the HL7 EHR system functional model?
It defines how to exchange data between the external systems and within the EHR itself according to the roles of data exchange process participants.
What does health interoperability with HL7 refer to?
It refers to leveraging common data exchange and stage strategies for achieving interoperability using HL7 and FHIR — the newest standard of the HL7 organization.






